25 Aug Sleep and Chronic Pain
Sleep and Chronic Pain
Sleep is important. More than important, it is as essential. As essential as oxygen, food, and water. Without it, you will die. Losing a few hours of precious sleep will make you feel pretty ordinary, to completely dreadful the next day.
I know I am late to the party here. For anyone who knew me at University and in my 20’s, my mantra was, “I will sleep when I am dead.” I simply did not see it as an efficient use of my time. If I could sleep less, I would have more time to study, earn money, and see my family and friends. I hypothesised that 4 hours is plenty. Wrong.
David Klyne is a researcher at the University of Queensland trying to understand the physiology of pain. He notes, “What we now know is sleep is partly regulated by inflammation and also impacts inflammation”. Inflammation is heavily involved in so many diseases, disorders, and conditions including pain. Frequently people with chronic pain find it difficult to fall asleep, or sleep is often disrupted by long night awakenings from their sensitive tissues.
On the flip side of this, low-quality sleep can dial up your sensitivity levels, regulating your perception of pain. David notes where sleep is concerned “quality is more important than duration”.
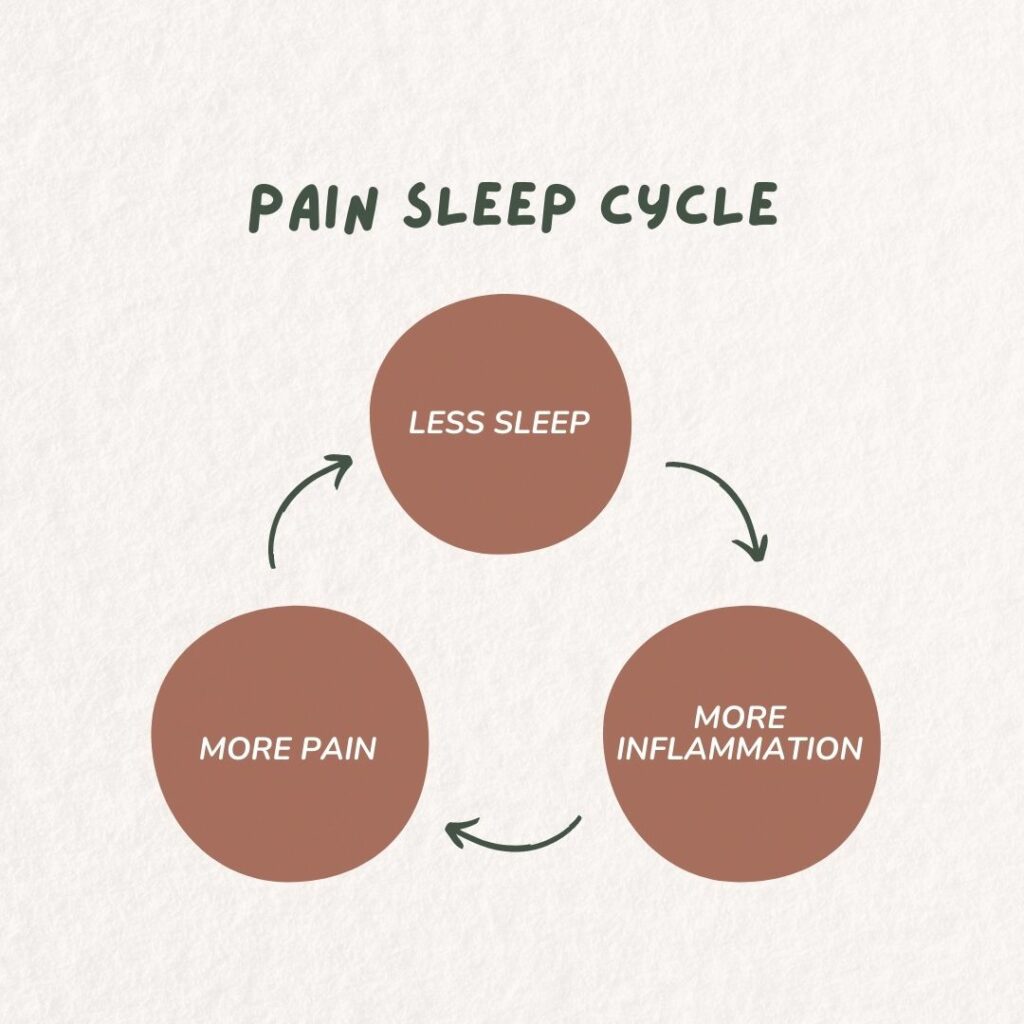
You see it is a circle; less sleep = more inflammation which = more pain = less sleep. But what comes first? The chicken or the egg?
Acute v Chronic Pain:
If you have had a long history of poor sleep your system may be primed for inflammation. In an acute pain situation where you stub your toe, what you are experiencing is inflammation in local nerves telling your brain you have just injured yourself and that you have pain. The chronic version of this, for example, the back pain you have had for 20 years, looks a little different. Eventually, the inflammation in the peripheral tissues, the area of the initial injury, is not as important anymore. The inflammation in the areas of the brain, associated with pain perception becomes the bigger problem.
To drop off to sleep our nervous system has to calm down. If you have chronic pain you have a much more active nervous system. This can mean it is hard to fall asleep or can interfere with how deep a sleep you get. It is normal to wake up multiple times a night, however, most people will roll over and go straight back to sleep without even realising it. People with chronic pain report waking up and noticing their pain leading to increased activity in their nervous system that has to calm down for them to get back to sleep.
Sleep and Hormones:
Reduced sleep directly affects your cortisol levels which can in turn raise your blood sugar levels. This might be something to consider if you have diabetes, struggling to get your blood sugar under control. Working on your sleep habits may be an important piece of the puzzle you are missing out on.
The positive impact of sleep:

How to improve your sleep:
Routine:
- Get up at the same time each morning regardless of the sleep you had the night before.
- Go to bed roughly around the same time each night
- Spend half an hour (a very active person may need longer than this) before bed, doing the same things in the same order each night, e.g. get things ready for the next day, have a shower, brush teeth, get into pyjamas then read a book. This helps the body learn to expect sleep and prepare for it. The last thing that you do in the routine must be quiet and relaxing. This is a wind-down time.
Only go to bed when you’re sleepy
Your sleep goes in waves throughout the night. Your energy levels also go in waves throughout the day. It is important to go to bed when the energy level is in a dip. Look for signs of sleepiness
Make the association between “bed” and “sleep” really strong
Your body learns to make associations all the time. We notice that our mouths salivate when we smell our favourite food cooking. Soon after smelling the food, we will get to eat it. Let us build up the association between bed and sleep, NOT a bed and other activities, or bed and stressing about not sleeping, or bed and pain.
Only use the bed for sleeping (and maybe one other thing….) ie. no reading books, watching tv, resting, eating. Find somewhere other than the bedroom to rest during the day. That also means no tossing and turning in bed feeling frustrated about being awake.
If it has been more than 20 mins (roughly) and you have not fallen asleep, get out of bed and do a quiet (non-stimulating) activity, until you feel sleepy and try again.
Relaxation
For the body to drop off to sleep, the nervous system needs to calm down. This can be achieved through involvement in calm non-stimulating activities, or through relaxation. You can find some relaxation techniques in our mindfulness and pain management module.
Relaxation techniques are particularly helpful when you are worried about not being able to sleep or about your pain. However, for it to work well when it is needed it needs to be practiced regularly. Maybe as part of your sleep routine, incorporate some meditation or breathing exercises.
Sleep Hygiene
- Diet: I think we all know this instinctively, low sugar, low fat, don’t eat right before bed, don’t drink 2L of water, and expect to sleep. Get off the booze.
- Total darkness for sleep time- eye masks, blackout blinds. The greater the difference between daytime light and evening darkness the more “melatonin” the body produces. This is a hormone that promotes sleep
- More light and sun during the day.
- Noise: Quiet is best. I have even tried earplugs. Calming noise like waves, rain, or white noise can be good and there are some great apps for this.
- Weighted blankets
- Exercise: Don’t exercise within 2-3 hours before going to bed, as it will increase the heart rate and body temperature making it harder to sleep
- Temperature: The core body temperature falls as we drop off to sleep. A warm shower in the evening is helpful as it will increase the body surface temperature initially, followed by cooling of the core body temperature
- Avoid napping: maybe only on the weekend or a special occasion, don’t make this a routine.

Professional Help
If you have breathing-related sleep problems such as obstructive or central sleep apnoea, your GP can help! They will either send you to a sleep clinic to do a test. I have heard after you are diagnosed, that some of these clinics may give you a sleep apnoea machine you can try free of charge to see if it helps you. If you can’t sleep because you are worrying about not sleeping, a clinical psychologist may be the best person to help empty all those thoughts rolling around in your busy mind.
Your Podiatrist
Hopefully, now you understand why we as podiatrists try to dig a little deeper when asking about the pain in your foot. If you are not sleeping, you are not giving your body a chance to heal and recover. So, if your mantra is “I’ll sleep when I am dead”, and you have chronic pain, it’s time to take a step back and think about the long-term damage you are doing and all the benefits you are missing out on!

Sorry, the comment form is closed at this time.